CURRENT SURGICAL STRATEGIES IN HEART FAILURE
CONVENTIONAL HEART SURGERY
Conventional heart surgery can be performed with acceptable risk and fairly good long-term results in well-selected patients (those with left ventricular failure, obstruction of coronary arteries, ischemic mitral incompetence and left ventricular aneurysm) with advanced heart failure. The results appear to depend mostly upon the quality and the amount of viable myocardium that can be improved by the procedure. Relatively, concerns arise as to the relative contribution of hibernating myocardium, ischemic mitral incompetence and left ventricular aneurysm or akinesia to left ventricular failure. It is anticipated that some patients will eventually need additional mechanical short or medium-term or even permanent mechanical support.
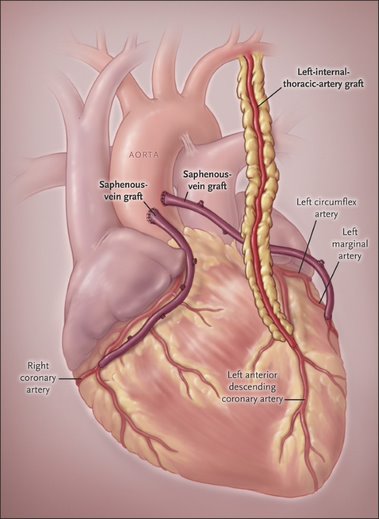
CORONARY REVASCULARIZATION
In heart failure from ischemic cardiomyopathy, revascularization is most effective in hibernating myocardium without cell death and without scarring. A good left ventricular wall thickness on echo (>8 mm) in the absence of infarct is a reliable indicator of viability. A high grade proximal coronary obstruction and good peripheral recipient vessel represent optimal conditions for bypass grafting.
Coronary artery disease with severely impaired left ventricular function is the main cause of heart failure in 27.5% of all patients considered for heart transplantation..
The surgical risk associated with coronary artery bypass grafting (CABG) in patients with ischemic cardiomyopathy has been substantially reduced in recent years thanks to the developments in cardiac surgery.
Whether a patient with ischemic cardiomyopathy will ultimately benefit from CABG in terms of survival and recovery of left ventricular function depends primarily on the presence of vital, revascularizable myocardial tissue (hibernating or stunned myocardium).
Different diagnostic methods are currently performed to assess myocardial viability such as fluorodeoxyglucose positron emission tomography, magnetic resonance imaging, single-photon emission computed tomography or echocardiography, to differentiate between stunned (still adequately perfused and metabolized), hibernating (mismatch between perfusion an metabolism, which is intact) and an infarction scar (neither perfused nor metabolized).
Therefore, the operative risk can be reduced with the help of preoperative patient screening and selection by myocardial viability assessment, and this selection process may extend the indication for CABG to those patients otherwise referred for heart transplantation.
VENTRICULAR RESTORATION
Left ventricular size is an important prognostic factor for long-term survival in patients with ischemic cardiomyopathy. Ventricular reconstruction is therefore an option for patients with ventricular dilatation and this could slow or present progressive heart failure in these patients. as in coronary revascularization, the decision as to whether perform ventricular reconstruction depends on the vitality of the remote myocardium and the size of the asynergistic area, since patients with large asynergistic areas of more than 35% of the total left ventricular volume are not suitable candidates for this procedure.
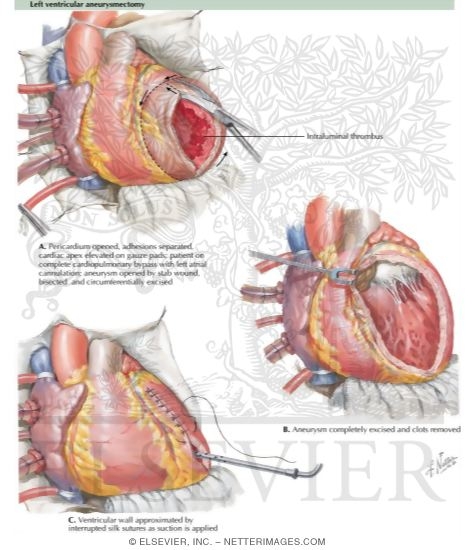
LEFT VENTRICULAR ANEURYSMECTOMY
This procedure is ideal when aneurysm is localized and thin-walled and when the other coronary artery systems are unaffected. Maximum improvement is obtained in patients with advanced heart failure. As with ventricular restoration, the value of ventricular volume reduction depends on the quality of the remaining myocardium.
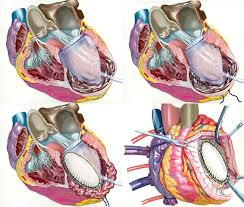
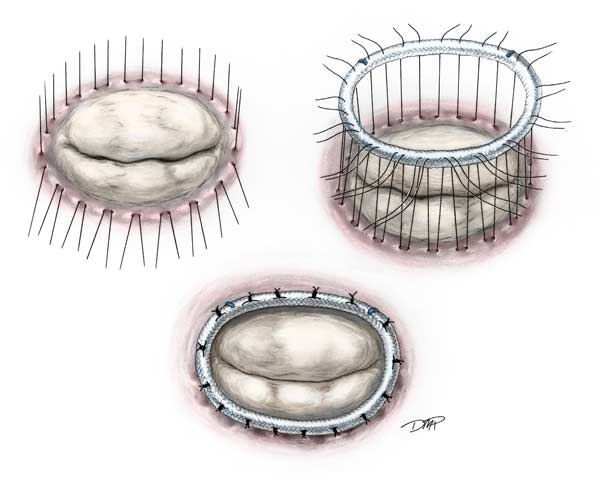
VALVE REPAIR FOR ISCHEMIC MITRAL INCOMPETENCE
Ischemic mitral incompetence (IMI) is the most important mitral valve disease of the future. Ventricular dilatation due to ventricular remodeling processes in heart failure often leads to mitral insufficiency, which in turn causes additional left ventricular stain and further exacerbation of symptoms. This is an unfavorable combination. Mitral valve repair is a therapeutic alternative, to reduce elevated myocardial load and left ventricular oxygen demands due to mitral insufficiency and thus improve left ventricular function. One surgical technique available in ischemic or dilated cardiomyopathy is annuloplasty using an undersized annuloplasty ring.
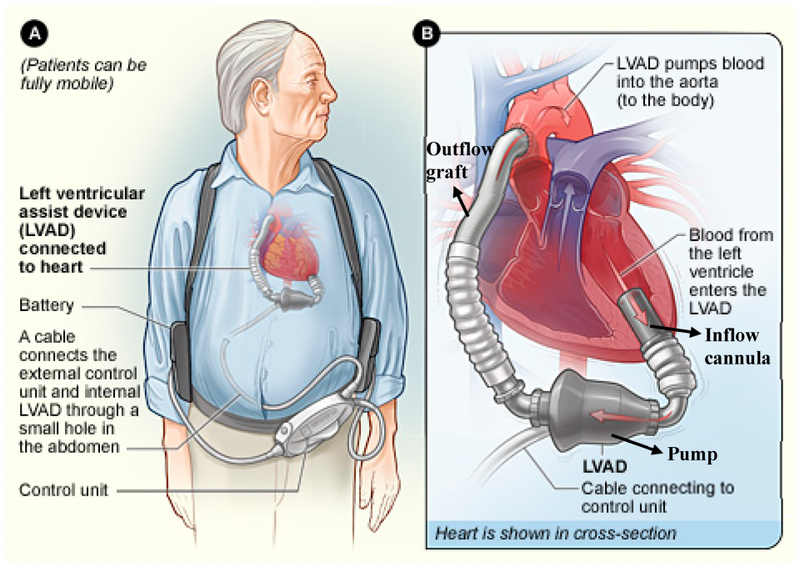
MECHANICAL CIRCULATORY SUPPORT
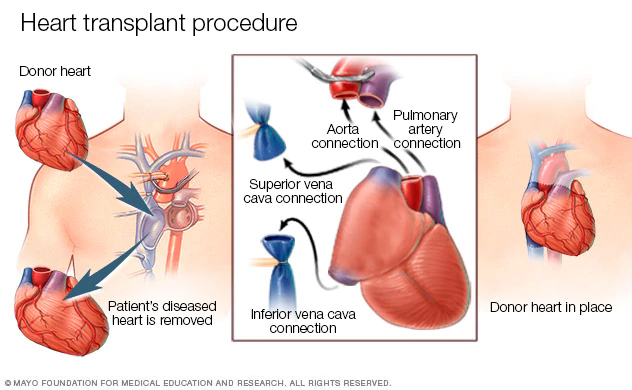
HEART TRANSPLANT